Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Pulmonary Embolism
Condition Basics
What is pulmonary embolism?
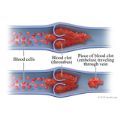
Pulmonary embolism is the sudden blockage of a major blood vessel (artery) in the lung, usually by a blood clot. In most cases, the clots are small and aren't deadly, but they can damage the lung. But if the clot is large and stops blood flow to the lung, it can be deadly.
What causes it?
Pulmonary embolism is caused by a blocked artery in the lungs. The most common cause of such a blockage is a blood clot that forms in a deep vein in the leg and travels to the lungs. Other things can block an artery, such as tumors or air bubbles. But these are rare.
What are the symptoms?
The most common symptoms of pulmonary embolism are sudden shortness of breath; sudden, sharp chest pain that may get worse when you cough or take a deep breath; and a cough. The cough may bring up blood or pink and foamy mucus.
How is it diagnosed?
Pulmonary embolism can be hard to diagnose. That's because the symptoms are like those of other problems, like a heart attack. A doctor will do a physical exam. You might have tests to look for blood clots or rule out other causes of your symptoms. Tests may include blood tests and a CT angiogram.
How is pulmonary embolism treated?
Doctors usually treat pulmonary embolism with anticoagulants (blood thinners). These medicines help prevent new clots and keep existing clots from growing. If symptoms are severe and life-threatening, "clot-busting" drugs may be used. They can dissolve clots fast. Another option is surgery or a less invasive procedure to remove the clot (embolectomy).
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Pulmonary embolism is caused by a blocked artery in the lungs. The most common cause of such a blockage is a blood clot that forms in a deep vein in the leg and travels to the lungs, where it gets lodged in a smaller lung artery. Clots in the deep veins of the arms or pelvis can also lead to a pulmonary embolism.
In rare cases, pulmonary embolism may be caused by other substances. They include:
- Small masses of infectious material.
- Fat. It can be released into the bloodstream after some types of bone fractures, surgery, trauma, or severe burns.
- Air bubbles or substances that get into the blood from trauma, surgery, or medical procedures.
- Tumors caused by rapidly growing cancer cells.
- Amniotic fluid.
Learn more
What Increases Your Risk
Many things increase your risk for having pulmonary embolism. These include:
- Being older than 40.
- Being overweight.
- Not taking anticoagulant medicine as prescribed.
- Having to stay in bed for more than 3 days (such as in a hospital stay).
- Sitting for a long time, especially when traveling long distances.
- Being pregnant, using hormonal birth control, or using hormone therapy.
- Having a recent surgery or injury that involved the legs, hips, belly, or brain.
- Having certain health problems. These include cancer, blood vessel disease, or an inherited clotting disorder.
- Smoking.
Prevention
If you've had pulmonary embolism once, you are more likely to have it again. Taking blood thinners reduces your risk.
You can also reduce your risk of pulmonary embolism by doing things that help prevent blood clots in your legs. For example:
- If you take blood thinners, take them just the way your doctor tells you to.
- Avoid sitting for long periods. Get up and walk around every hour or so, or flex your feet often.
- After an illness or surgery, try to get up and out of bed often. If you can't get out of bed, flex your feet every hour to keep the blood moving through your legs.
- Wear compression stockings if your doctor recommends them.
Symptoms
The most common symptoms of pulmonary embolism are:
- Sudden shortness of breath.
- Sudden, sharp chest pain that may get worse when you breathe deeply or cough.
- A cough. The cough may bring up blood or pink, foamy mucus.
Pulmonary embolism can also cause other symptoms. These include:
- A fast heart rate.
- Wheezing.
- Fainting.
If you have symptoms like these, you need to see a doctor right away, especially if they're sudden and severe. Quick treatment could save your life or reduce the risk of future problems.
What Happens
Symptoms of pulmonary embolism usually begin all of a sudden. Reduced blood flow to one or both lungs can cause shortness of breath and a rapid heart rate. Inflammation of the tissue that covers the lungs and chest wall (pleura) can cause sharp chest pain.
A blood clot reduces the blood flow and may cause damage to lung tissue. The blood clot might dissolve on its own. If it does, it may not cause any major problems. But without treatment, new clots can form and cause another pulmonary embolism. If pulmonary embolism is diagnosed right away, treatment with anticoagulant medicines may prevent new blood clots from forming.
If a blood clot blocks the artery in the lung, blood flow may be completely stopped, causing sudden death. Doctors will consider aggressive steps when they are treating a large, dangerous pulmonary embolism.
When to Call a Doctor
Call 911 or other emergency services immediately if you think you have symptoms of pulmonary embolism.
Symptoms include:
- Sudden shortness of breath.
- Sudden, sharp chest pain that may get worse when you breathe deeply or cough.
- A cough. The cough may bring up blood or pink, foamy mucus.
- A fast heart rate.
- Wheezing.
- Fainting.
Call your doctor now if you have symptoms of a blood clot in the leg, including:
- Swelling, warmth, or tenderness in the soft tissues of your leg. Swelling may also appear as a swollen ridge along a blood vessel that you can feel.
- Pain in your leg that gets worse when you stand or walk. This is especially important if there is also swelling or redness in your leg.
Blood clots in the deep veins of the leg are the most common cause of pulmonary embolism.
Exams and Tests
It may be hard to diagnose pulmonary embolism. That's because the symptoms are like those of many other problems, such as a heart attack or pneumonia.
A doctor will do a physical exam and ask questions about your past health and your symptoms.
You might have tests to look for blood clots or to rule out other causes of your symptoms. Tests may include:
- A chest X-ray. This may rule out an enlarged heart or pneumonia.
- Electrocardiogram (EKG). This may help rule out a possible heart attack.
- Blood tests, such as a D-dimer. D-dimer levels are usually high in people with pulmonary embolism.
- A CT scan or CT angiogram. These tests can look for pulmonary embolism or for a blood clot that may cause it.
- A ventilation-perfusion lung scan. This test scans for abnormal blood flow through the lungs.
Learn more
Treatment Overview
Doctors usually treat pulmonary embolism with medicines called anticoagulants. They are often called blood thinners, but they don't really thin the blood. They help prevent new clots and keep existing clots from growing.
Most people take a blood thinner for a few months. People at high risk for blood clots may take it for the rest of their lives.
If symptoms are severe and life-threatening, "clot-busting" drugs called thrombolytics may be used. These medicines can dissolve clots quickly, but they increase the risk of serious bleeding. Another option is surgery or a less invasive procedure to remove the clot (embolectomy).
Some people may have a filter put into the large vein (vena cava) that carries blood from the lower body to the heart. A vena cava filter may help keep blood clots from reaching the lungs. This filter might be used if you can't take an anticoagulant.
Learn more
Self-Care
- Take your medicines exactly as prescribed. Call your doctor if you think you are having a problem with your medicine. You will get more details on the specific medicines your doctor prescribes.
- If you are taking a blood thinner, be sure you get instructions about how to take your medicine safely. Blood thinners can cause serious bleeding problems.
- Try to walk several times a day. Walking helps keep blood moving in your legs. Before doing other types of exercise, ask your doctor what type and level of exercise is safe for you.
- Take steps to help prevent blood clots in your legs. For example:
- Exercise your lower leg muscles if you sit for long periods of time. Pump your feet up and down by pulling your toes up toward your knees then pointing them down. Repeat.
- After an illness or surgery, try to get up and out of bed often. If you can't get out of bed, flex your feet every hour to keep the blood moving through your legs.
- Take plenty of breaks when you travel. On long car trips, stop the car and walk around every hour or so. On the bus, plane, or train, get out of your seat and walk up and down the aisle every hour, if you can.
- Wear compression stockings if your doctor recommends them.
- Check with your doctor about whether you should use hormonal forms of birth control or hormone therapy. These may increase your risk of blood clots.
- Have a healthy lifestyle. This includes being active, staying at a healthy weight, and not smoking.
- Get vaccinated against COVID-19, the flu, and pneumonia.
Learn more
Medicines
Medicines called anticoagulants are used to treat pulmonary embolism. Anticoagulants are also called blood thinners. They can help prevent new blood clots and keep existing clots from growing.
You'll likely take an anticoagulant for at least 3 months. You may take it longer. If your risk for another pulmonary embolism stays high, you might take it for the rest of your life.
Different types of anticoagulants are used. Talk with your doctor about which medicine is right for you.
If you are in the hospital, you might be given an anticoagulant as a pill, a shot, or in a vein through an I.V. After you go home, you might give yourself shots for a few days. For the long term, you'll likely take a pill.
Clot-dissolving (thrombolytic) medicines aren't often used to treat pulmonary embolism. They can quickly dissolve a blood clot. But they also greatly increase the risk of serious bleeding.
Learn more
Surgery
To improve blood flow, a blood clot can be removed during surgery. Or the clot might be removed with a less invasive procedure that uses a catheter (a thin tube that's guided through a blood vessel). This surgery or procedure is called an embolectomy.
An embolectomy is not common. But it may be done for a few reasons. These include:
- You can't have thrombolytic treatment.
- The clot is so dangerous that you can't wait for medicine to work.
- You've had thrombolytic treatment, but it hasn't worked well enough.
Related Information
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.